How is breast cancer detected?
Detection
Breast cancer is common in women. That is why knowledge about the warning signs is so important. On average, a woman has a one in eight chance of developing breast cancer during her lifetime. In men, breast cancer is rare, but they should remain equally alert for unusual changes in a breast. Also transwomen have an increased risk.
The most common alarm sign is a lump in the breast that you never noticed before. Less frequent but also suspicious are any skin changes to a breast (a dent, redness, eczema or flaking), a retracted nipple or discharge from the nipple. Furthermore, a heavy feeling, a hard disc, painful or otherwise, a lump in the armpit should ring an alarm bell. Almost always, these changes occur in one breast. Do you notice anything unusual? Then don't wait and make an appointment with your doctor or gynecologist.
Mammography
Your family doctor or gynecologist will examine your breasts, and if he confirms your suspicion, he will refer you to a radiology center for a mammogram. A mammogram consists of multiple x-rays of both breasts. This examination may feel uncomfortable for a while because the breast is compressed. Count to ten and you'll be off the hook. A mammogram can detect lesions up to five times smaller than what you can feel yourself.
Another way to detect breast cancer is through the breast cancer screening program. This is done through a screening mammography (same examination as a mammogram, but in the absence of alarm signs). Even if you don't detect suspicious changes in a breast, every woman between the ages of 50 and 69 is invited for a free screening mammogram every two years. The age limits used here have to do with the risk of breast cancer. This is highest in those over 50. The fact that the screening is no longer free from the age of 70has economic reasons and does not mean that you can no longer get breast cancer. It is good to have your breasts checked regularly beyond that age. You then pay a small fee for the mammogram, which is largely refundable at all ages.
Participation in population screening is not mandatory. It has both advantages and disadvantages. The main advantage is that a possible breast cancer can be detected earlier, which is always beneficial for survival. The disadvantage is that there is a risk of overdiagnosis. Sometimes abnormal cells are found in the milk ducts, which would never grow into an actual breast cancer. This is called DCIS or in full Ductal Carcinoma In Situ. They are an early stage of breast cancer. Some precursors evolve into breast cancer and some do not, but we cannot make that distinction today. That is why they are all treated.
When a mammogram is normal, no further action is needed.
Further research
In the event of an abnormal result from your mammogram, whether you felt something suspicious yourself or participated in the population screening with screening mammography, you will always be referred for additional testing at an accredited breast clinic.
Sometimes additional mammograms are done and usually an ultrasound is also done to further assess the suspicious spot. An ultrasound, which uses sound waves, can distinguish between a solid tumor and a cyst. Cysts are generally benign.
Next, the doctor takes a biopsy of the suspicious area. To do this, he pricks cells from the suspicious area with a thin, hollow needle that are sent to the laboratory for cell testing. The examination of these cells checks whether malignant cells are present. If so, a second biopsy follows in which a larger piece of suspicious tissue is removed through a different type of needle under local anesthesia. That piece also goes to the lab, where they examine whether the malignant cells are affecting the surrounding healthy cells. When that is the case, you can speak of breast cancer. To be considered breast cancer, a lump must meet three conditions: the presence of malignant cells, damage to surrounding healthy tissue and the possibility of these cells spreading to other parts of the body.
Laboratory tests combined with imaging such as an MRI scan, a CT or PET scan and sometimes sentinel lymph node examination (examination of the lymph nodes in the armpit) or a bone scan, allow us to determine what type of cancer is involved and whether the cancer has spread to lymph nodes or other organs. In this way, your breast cancer is precisely identified by type, size and extensiveness (stage). There are untold variations possible and that determines which treatment gives you the best chances.

Breast cancer screening pros and cons

Did you feel a lump?

Look at your breasts a little more often

Breast cancer screening: join in, it could save your life

More breast cancer awareness, less breast cancer

The look and feel of your breasts

10 questions about screening mammography

Screening reduces breast cancer mortality in Belgium
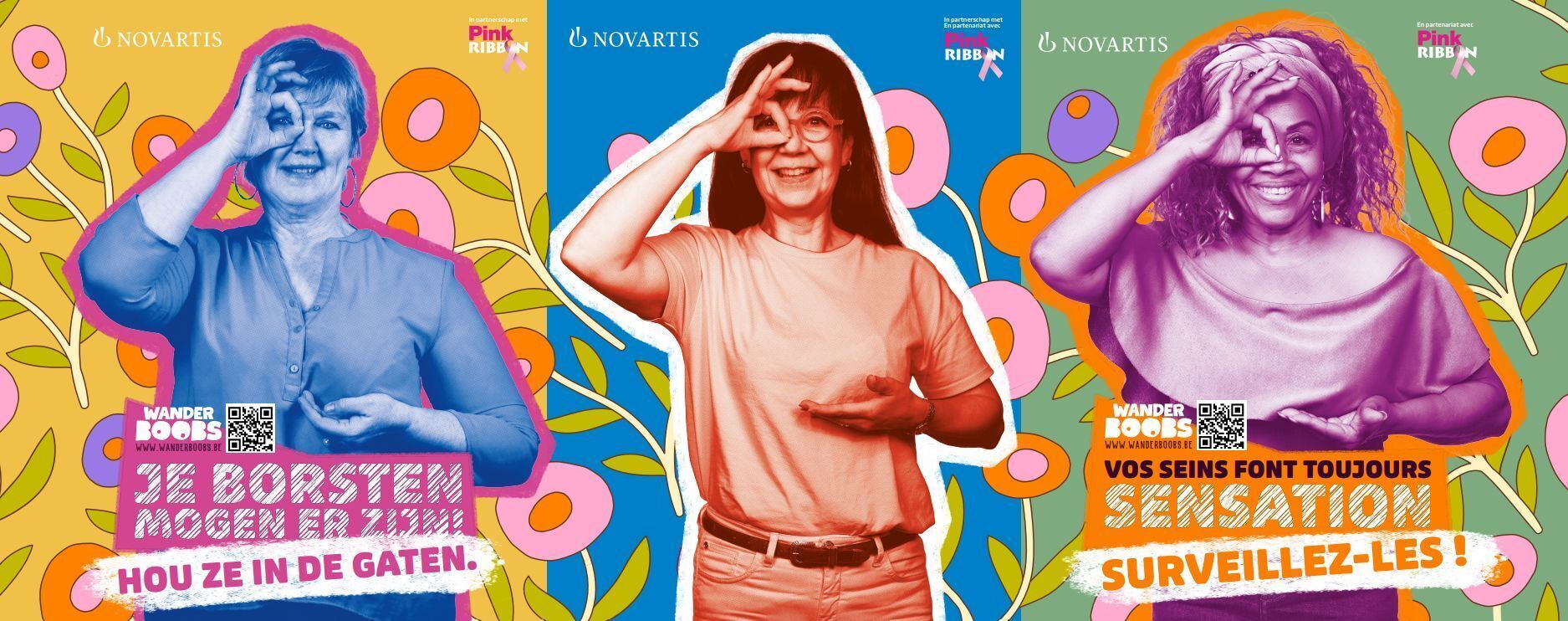
Novartis and Pink Ribbon launch Wander Boobs campaign

The alarm signals of breast cancer: Do you know all 9 of them?

Breast cancer screening stops at 69. And then?
We could not find any results matching your search terms.
Try another search term and/or filters or contact us and we will help you further.

Editor in Chief Pink Ribbon


























